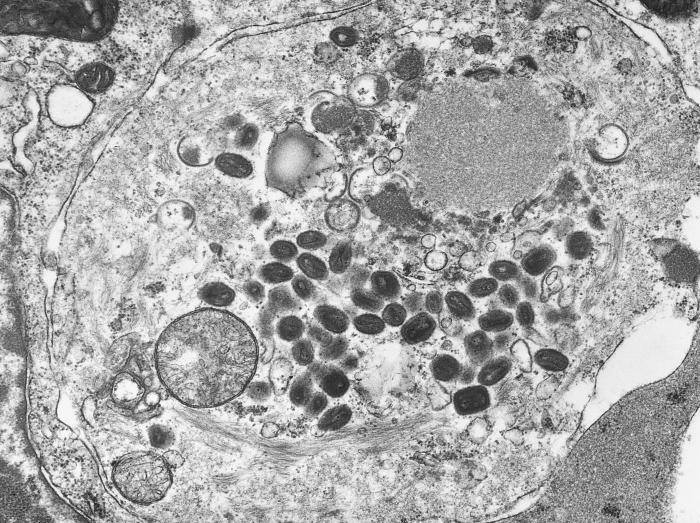
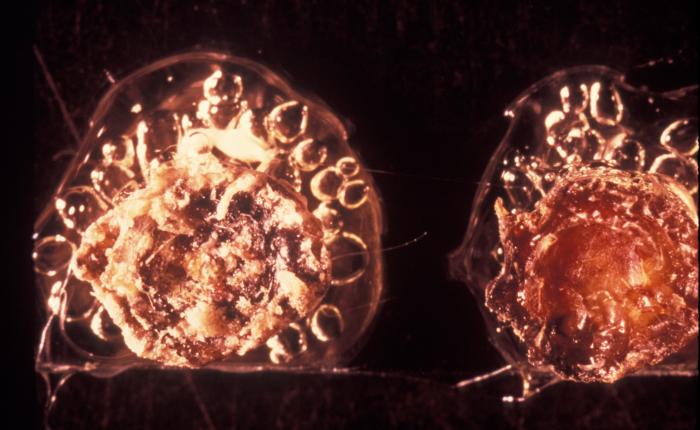
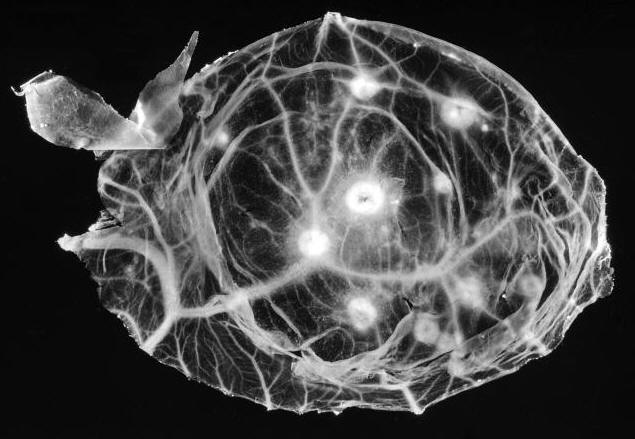
Smallpox VirusOverview: Smallpox is a highly contagious infection caused by the enveloped, doubled-stranded DNA virus smallpox, also known as variola virus (Figure 1). The virus ranges in size from 200 nm (nanometres) to 400 nm and possesses a genome that is 200 kilobase pairs long, making it one of the largest animal viruses. The pathogen is pleomorphic and contains a nucleocapsid that is typically dumbbell-shaped. Membrane proteins are arranged helically, and are used to attach to host membrane receptors to initiate entry. The pathogen belongs to the genus Orthopoxvirus and the family Poxviridae. Smallpox virus has two main variants, namely, variola major and variola minor, both of which infect humans only. Variola major is the causative agent of the deadly infectious disease, while variola minor is a much less common variant that produces mild, non-fatal symptoms. The disease is commonly spread by close interaction with an infected person via the inhalation of virion-contaminated aerosols. During the infection, substantial amounts of the virus are also found in the spleen, kidneys, bone marrow, lymph nodes, and other viscera. Figure 1. A transmission electron micrograph of a tissue section containing variola viruses. Transmission: The usual entry of smallpox virus is through the respiratory tract with infection of the oropharyngeal (mouth) or respiratory (trachea and lung) mucosa. Secretions from the mouth and nose, rather than scab material, are the most important source of human-to-human transmission. The initial infection in the oropharynx or respiratory tract produces neither symptoms nor local lesions, and patients are not infectious until an oropharyngeal enanthem appears at the end of the primary incubation period. Transmission to others is generally through coughing out of virions in oropharyngeal secretions. Patients are most infectious during the first week of rash. Scab material forms as the rash dries and usually consists of large fragments of cellular debris, with virions bound within a dense, fibrous mesh containing a large amount of the antiviral substance interferon. Infectious virus is difficult to release from scabs except by mechanical grinding. Pathogenicity: There are two slightly different virions of variola that are morphologically distinct, called the intracellular mature virion (IMV) and the extracellular enveloped virus (EEV). These virions are surrounded by different numbers of membranes, they have different proteins on their surface, and they bind to different cell receptors, which causes some confusion on how exactly the variola virus enters the host cell. The majority of IMV remain intracellular until cell lysis, but some become wrapped by additional membranes during a complex morphogenesis pathway to form intracellular enveloped virus (IEV). IEV are transported on microtubules to the cell surface, where they fuse with the plasma membrane to expose a virion on the cell surface. This virion may be retained on the cell surface as cell-associated enveloped virus or released as EEV. The binding proteins and their functions for variola virus are unknown, however it has been determined that only the IMV virion has the proteins needed for fusion to the cell. In this case, it is deduced that the outer layer of an EEV is discarded before fusion to the host cell. The specific entry path of the virion depends on the virus strain or type; the virus may enter the cell through either fusion at the plasma membrane or through the endosomal pathway. Finally, immediately before entering the cell the outer membrane of the virion is shed, which leaves only the dumbbell-shaped core to enter the host cell. Once the virus enters into the cell, a host RNA polymerase is activated. Along with other accessory enzymes, this polymerase begins to be translated by the host cell. This leads to the uncoating of the virus. The dumbbell-shaped core of the virus is revealed by the early mRNA. The nucleoproteins pass through the core wall making it disappear. The uncoating is a process completed by RNA and protein synthesis. The DNA within the variola virion is cut in half by the enzyme helicase. DNA polymerase then matches the strand with each unique pair, therefore creating a new strand of identical DNA for the progeny virion. Once all the essential proteins are transcribe and translated, progeny virions are assembled. Infection of the host cell typically results in about 10000 copies of the genome per cell. Symptoms: General symptom of the infection are lesions on the skin (Figure 2). Other symptoms include high fever, fatigue, backache, and other flu-like symptoms. An individual will remain symptom free for the first 10 to 12 days. After this period, the virus spreads throughout the body causing the onset of the fever and rash. After the first week, the virus is released through the respiratory tract. An individual is most contagious when a rash and fever have developed during the first week, when the virus is released via the respiratory tract. In the later stage of the disease when the scabs start to fall off, the individual is only moderately contagious since the shed skin is not highly infectious. However, the virus can remain stable for 2 to 4 months on scabs and can remain on clothing for months to years. During the incubation period, a person cannot infect another. Figure 2. This infant was infected with the smallpox virus, and on day four of the rash, shows the typical lesions on his hand and forearm. Identification: Smallpox can be identified through various microscopic and laboratory diagnosis. Smallpox can also be differentiated from such viruses such as chickenpox via comparative morphology of the scabs. For instance, unlike smallpox, chickenpox lesions are superficial, and on any one part of the body there are lesions in different stages (i.e.: papules, vesicles, and crusts) (Figure 3). Also, chickenpox rarely has lesions on the palms and soles, which is not the case with smallpox. Initially the characteristic lesions first appear on the head, then on the rear trunk, and then the extremities. Figure 3. This is a chickenpox scab (left), and smallpox scab (right) viewed from above as a demonstration in comparative morphology. At the microscopic level, Poxviruses form cytoplasmic inclusions, such as Guarnieri bodies in virus-infected epidermal cells. Generally, small particles of insoluble substances (i.e. lipids or calcium oxalate) suspended in the cytosol are often referred to as cytoplasmic inclusions. Microscopically, the virus appears as pink blobs when stained with eosin and hematoxylin (Riedel, 2005). In order to precisely diagnose a smallpox infection, virus must be grown on chorioallantoic membrane - a vascular membrane found in bird eggs - and then have the lesions examined (Figure 4). The polymerase chain reaction and restriction fragment length polymorphism analysis are also used to identify the specific strains, while ELISA and serologic tests measure the variola virus-specific immunoglobin and antigen to aid in the diagnosis of the virus. Figure 4. A photograph revealing smallpox virus pocks on the chorioallantoic membrane of a developing embryonic chick. Poxviruses are very easy to isolate, and will grow in a variety of cell cultures, producing characteristic hemorrhagic pocks on the chick chorioallantoic membrane. Prevention: Smallpox vaccination will prevent or significantly lessen the severity of smallpox symptoms in the vast majority of people. Vaccination four to seven days after the exposure to smallpox virus will likely offer some protection from disease or modify the severity of disease. References: Riedel, S. (2005). Smallpox and biological warfare: a disease revisited. Baylor University Medical Center Proceedings, 18: 13-20. |
 In fact, both musicians contracted and survived the disease as children; both had visible pockmark scars on their faces. In fact, both musicians contracted and survived the disease as children; both had visible pockmark scars on their faces.
|